Robohub.org
Developing cost-effective, capable, surgical robots with a sense of “touch”

Maj. (Dr.) George Kallingal showcases a robotic surgical system while Lt. Col. (Dr.) Thomas Novak, Brooke Army Medical Center’s chief of pediatric urology, looks on at San Antonio Military Medical Center in San Antonio. Photo by Robert Shields
This article was first published on IEC e-tech.
Robotic‑assisted surgery involves a surgeon using a computer‑assisted electro‑mechanical device to carry out complex and technically demanding medical procedures on a patient. The value of surgical robotic tools lies in their role as machines that extend the capabilities and precision of the surgeon, rather than replacing human skills.
Typically, a robotic surgical system includes a camera arm and multiple mechanical arms with surgical instruments attached to them. The surgeon controls the arms while seated at a computer console which is located close to the operating table and provides a high‑definition, magnified, 3‑D image of the surgical site. The surgical robot’s computer software also filters out the surgeon’s hand tremors. For robotic radiosurgery, non‑invasive technology can deliver high‑precision radiation therapy using continual image guidance technology and computer‑controlled robotic mobility.
Robotic surgical technology enables a surgeon to perform surgical movements that exceed the natural range of motion of the human hand with greater precision, combined with high definition 3‑D visualization and magnification. Smaller incisions mean smaller scars, less blood loss and reduced trauma to the tissue that is a feature of regular surgery.
The smooth operation of a surgical robot relies on its electrical and mechanical components, sensors and computer software working together in harmony combined with the skill and experience of the surgeon in charge.
IEC Standards vital as market expands
Growth in the worldwide robotic surgical systems market is being fuelled as emerging competitors challenge the dominance of established players by offering greater affordability and technological innovation.
Global sales of surgical robotic systems are projected to reach $28.8 billion by 2020, according to a 2016 report by US research consultancy Allied Market Research (AMR). According to AMR, the increased adoption of advanced robotic surgery over conventional open surgery, a growing number of surgical procedures and the rise in gynaecological, neurological and urological disorders are the major factors that will boost market growth. As a result, the surgical robotic procedures market is estimated to grow at a compound annual growth rate (CAGR) of 4.9% during 2015‑2020, fostering the growth of the surgical robotics market, the report adds.
Gynaecology applications comprised the largest share of the surgical robotic systems market in 2014 (28%), and orthopaedic surgery, currently at 22%, is projected to be the fastest growing application segment during the forecast period. North America and Europe collectively account for around four-fifths of worldwide surgical robotic systems market revenue, but Asia-Pacific’s share is expected to grow rapidly owing to a growing awareness of robotic surgeries and increasing healthcare expenditure, AMR concluded.
Medical robotics is a relatively new domain and relies on IEC International Standards to help ensure that the design and manufacture of parts meet the strictest requirements. The SCs (Subcommittees) and WGs (Working Groups) of IEC TC 62: Electrical equipment in medical practice, have been responsible for carrying out the bulk of the medical equipment standardization work required to produce the IEC 60601 family of standards. These cover the safety requirements for ME (medical electrical) equipment and MES (medical electrical systems) in current use.
IEC SC 62A: Common aspects of electrical equipment used in medical practice, formed Joint Working Group (JWG) 9 with ISO TC 184/SC 2 in June 2011. JWG 9’s remit is to “develop general requirements and guidance related to the safety of medical electrical equipment and systems that utilize robotic technology. The work encompasses medical applications (including aids for the disabled) covering invasive and non‑invasive procedures such as surgery, rehabilitation therapy, imaging and other robots for medical diagnosis and treatment”.
More than 80 experts are currently active in SC 62A/JWG 9, reflecting the importance of standardization for the sector. The IEC is also examining the still new and rapidly evolving issue of the incorporation of higher levels of autonomy in ME equipment and MES.
Touch me, heal me
Surgical robots incorporate sensors, for example, to relay information or allow the precise application of force. Manufacturers can build more reliable, efficient and safe sensors and microelectromechanical systems (MEMS) thanks to International Standards prepared by IEC Technical Committee (TC) 47: Semiconductor devices and IEC Subcommittee (SC) 47F: Microelectromechanical systems.
New types of motors for surgical robots use ceramics and plastics rather than metal components, so robots using these materials would not be affected by machines that emit magnetic waves, such as Magnetic Resonance Imaging (MRI) scanners.
As robots become cheaper and more capable and the costs of sensors and software that heighten their capability continue to fall, new medical applications are expanding.
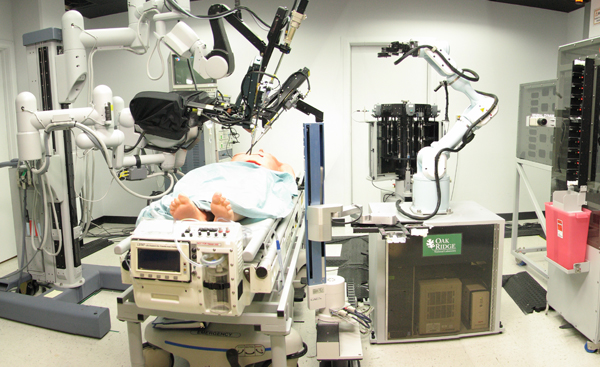
The SRI-led Trauma Pod, developed for DARPA as a next-generation mobile robotic surgery platform for the military. Credit: SRI International via Wikimedia Commons
Minimally invasive robot instruments can both look and feel for cancer deep within the body, using a combined ultrasound probe and pressure sensor array. The latest radiation oncology robotic surgery devices, systems and instruments manage cancer surgery through radiation excision that eliminates open cutting in the body. Meanwhile, advances in robot‑assisted hip replacement surgery assist surgeons in ensuring optimal alignment of artificial hip joints.
The next generation of robotic-assisted tools for surgeons includes advanced imaging and sensors to help doctors during operations. Researchers at Harvard are developing low‑cost, millimetre‑scale force sensors for robotic surgical tools, where size is the biggest challenge, with the aim of eventually providing surgical robots with a sense of “touch”.
Other innovations include robotic suturing, a robot‑guided laser bone‑cutting device which offers more precise cutting geometries, and miniature snake‑like robots only a few millimetres in diameter.
A team led by the Hong Kong Polytechnic University is developing what it describes as the world’s first internally motorized minimally invasive surgical robotic system, and successfully carried out trials on animals using the prototype in December 2015.
The system, called the Novel Surgical Robotic System (NSRS), can be inserted through a single, small incision or even a natural orifice (incision‑less) and expanded inside the human body to perform various surgical operations. The small arms and micro‑motors that control them are then able to work on the body without requiring a large external machine to drive the tools.
The system is capable of haptic (tactile) feedback, allowing the surgeon operating it to feel the stiffness of tissues manipulated by the instruments, a feature not available on current major robotic surgical systems.
Dr Louis Phee of Singapore’s Nanyang Technological University foresees a time when customizable micro/nano self‑configurable robots will be used for screening, surgery and biopsies. Nano‑robots are robots the size of a cell that could be introduced in blood flow to eliminate cancer cells or for tissue repair, among other uses.
Nanotechnology, the manipulation of matter on atomic and molecular scales, is a rapidly growing technology, but one that is still, to a great extent, in a developmental phase. However, it is seen as having great potential in medical applications. IEC TC 113 prepares International Standards for nanotechnology.
Dr Phee argues that “the real challenge for the future of robotics in surgery (and perhaps for surgery in general) is to go beyond the mere imitation and substitution by a robot of conventional procedures and surgical gestures, and rather to explore completely novel procedures that are possible only by means of robotic/mechatronic tools together with human surgeons.”
Robot love
Medical robots have wider applications beyond just surgery. For instance, robotic arms provide rehabilitation therapy for patients recovering from strokes and other neurological disorders. Autonomous mobile robot fleets can serve as medical workhorses, travelling for miles along hospital corridors carrying medical supplies, patients’ meals and other goods.
With people around the world living longer, and rising healthcare costs for the elderly overtaking tax revenues in many developed countries, one solution being mooted is that “cyberconscious” robots could replace human caregivers. In this scenario, care‑giving robots would assist their elderly charges with everyday tasks and remind them to take their medication.
The latest research extends to whether robots could make stronger social and emotional connections with people. The next generation of home‑care robots, for instance, could use visual cues such as tears, audio signals such as extended silence or barely audible speech, and physiological signs such as lowered temperature and raised blood pressure to assess moods among the elderly and cheer them up during periods of unhappiness.
tags: c-Health-Medicine, surgical robotics